Parasol International 19th Annual Anniversary Dinner

29 November was the date chosen for the 19th anniversary Parasol International dinner. This year Ruth Monicka Parasol, principal benefactress of The Parasol Foundation was determined that the 140 plus guests from the Gibraltar business and wider community should hear firsthand about the work that Parasol Foundation supports. The focus this year was on women’s health; the complex challenge of trying to prevent premature births, and advancing our understanding about ovarian cancer which has limited treatments and very poor outcomes.
So, we had three powerful contributions from three powerful women who are @Parasol Foundation research fellows. Dr Lynne Sykes, Dr Paula Cunnea and Dr Shira Peleg Hasson.
Dr Lynne Sykes - Reducing Premature Births
First, Dr Lynne Sykes, Clinical Senior Lecturer, is part of The Parasol Foundation Centre For Women’s Health and Cancer Research, established in 2022. It’s a partnership with Imperial Health Charity and Imperial College Healthcare NHS Trust. The Centre has twin aims - to improve women’s health and enable women to pursue successful careers in research and STEM fields.
Dr Sykes’s goal is clear - to stop the one in ten women who give birth prematurely. There are complex factors at play but the most common cause of very early premature births is the presence of certain ‘risky’ bacteria in the vagina in combination with a heightened immune response in the mother. Imagine if you could predict who was likely to have the risky bacteria and the heightened immune response from the mother, then you could develop a treatment to change both. Guess what? Lynne and her colleagues at Imperial College London have developed a test that takes just three minutes to provide a personalised bacterial and immune profile. Furthermore, in a pilot study, they have found that using a specific vaginal pessary with the ‘good’ bacteria can change the mother’s profile from the risky to the good bacteria, AND it dampens down the mother’s immune response. Initial results also point to a REDUCTION in premature births. The next stage is to progress to a full-scale clinical trial and see if these highly promising results are replicated at scale. If they can, then this could be the most significant advance in preterm birth PREVENTION for 80 years.
Dr Paula Cunnea – A Brighter Future For Women With Ovarian Cancer
Dr Paula Cunnea, Ovarian Cancer Research Fellow shared her work which is also part of the Parasol Foundation Centre. 1 in 50 women will be diagnosed with ovarian cancer in their lifetimes. 7,300 women are diagnosed every year in the UK alone. Less than half of women diagnosed survive more than five years compared to 90% of breast and prostate cancer. Dr Cunnea and her team want to change those numbers for all women.
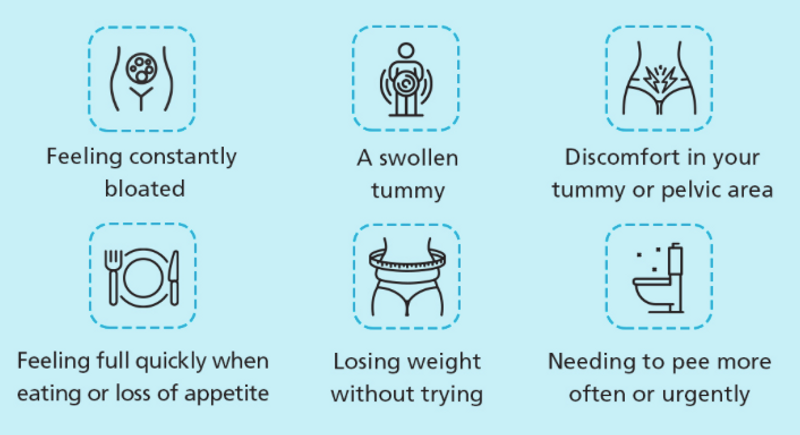
But it’s a huge challenge. Ovarian cancer’s share of all UK research funding has halved. Most women are diagnosed too late, once the cancer has spread. One in five UK women mistakenly think that the cervical screening programme would detect ovarian cancer too! Combine these issues with the fact that the six symptoms (see graphic) are vague and can also indicate other illnesses and you can see how hard it is to make progress. But Paula and her team with the renowned gynae-oncology surgeon Professor Christina Fotopoulou are making progress. Ovarian cancer is not one disease it is many. Their focus is on high grade serous ovarian cancer as it is the most prevalent and lethal type of ovarian cancer. They are working on understanding why some patients and their tumours become resistant to chemotherapy and a newer therapy called PARP inhibitors; how tumours spread to different parts of the abdomen and study how they behave to understand the evolution of the disease and develop new biomarkers and drug treatments.
They are very fortunate to be working alongside Christina who conducts maximal effort cytoreductive surgery to save her patients’ lives. That gives the research team access to different tumours that they can research in the laboratory. Painstaking, precise work has led to the development of 3D models of ovarian cancer to mimic tumour behaviour; a drug under development to combat chemotherapy and PARP inhibitor resistance and thirdly investigation of the variability of tumours has led to deeper understanding of the disease. As many as 1 in 5 patients can have variability in a biomarker used to stratify patients for treatment. This means that patients need to be treated as individuals to find the best treatment that is likely to work for them.
Paula and her team are bringing hope to thousands of women and feel that there is room for optimism that in the future more women will survive for five years or more.
Dr Shira Peleg Hasson – Latest Gynecological Cancer Research Findings
Finally, Dr Shira Peleg Hasson, a medical oncologist consultant and cancer researcher from Tel Aviv Sourasky medical centre and clinical research fellow at The Royal Marsden Foundation Trust, who is funded through the Icholov Programme, shared some of her research findings and ongoing projects.
Dr Peleg Hasson’s research focus is patients with gynaecological malignancies (cancers of the cervix, uterus and ovaries). These particular cancers make up 15% of the estimated 9.2 million new cancer cases in females worldwide. Beyond the high numbers of cases, these cancers place a heavy burden and have a profound impact on the quality of life of the affected women and their families.
However, out of 18 cancers that attracted $24bn from public and philanthropic grants in four years, prostate cancer secures the most funding and gynaecological cancers are in the lower half of the funding allocation. There is funding inequity for research into women’s cancers which needs to be addressed promptly so women’s cancers don’t fall further behind and in the interim it makes the support of the Foundation more valuable in this area.
One of her research projects at the Royal Marsden focuses on low grade serous ovarian cancer as that is rare and affects young women. Her work aims to identify biomarkers and genetic mutations within tumours and multiple blood samples (liquid biopsies) over time. In time, this should enable the team to develop a more personalised treatment approach and crucially non-invasive ways to treat early disease relapse, monitor disease treatment and guide clinicians’ decisions on treatments, ultimately leading to better outcomes and quality of life for patients with low grade ovarian cancer.
Medical cannabis use is another area of interesting research. Many countries now include medical cannabis in their therapeutic arsenal to manage symptoms related to cancer diagnosis as well as the side-effects of some treatments. Shira has led a study which has looked at the safety of integrating medical cannabis alongside standard care treatment for ovarian cancer, to guide evidence-based protocols for its use. The study findings which are due for publication in a prestigious journal shortly suggest that it doesn’t interfere with the efficacy of standard of care treatments so that should give the green light for its use which could benefit patients’ quality of life.
We will keep a close eye on the research programmes and the promise they hold for better treatments for these under-served cancers.
